Renagel
"Order renagel 800 mg amex, gastritis elimination diet".
By: X. Jared, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D.
Clinical Director, Harvard Medical School
Unfortunately gastritis diet èãðè cheap renagel 400 mg free shipping, some malignancies recur many years after apparently successful control gastritis symptoms heart cheap 400 mg renagel free shipping. The second measure of success is resumption of a normal life pattern without sequelae from the disease or its treatment chronic superficial gastritis definition discount renagel american express. However gastritis diet ãèäîíëàéí discount renagel 400mg on-line, these patients require long-term follow-up for reasons other than cancer recurrence. In addition to the physical, social, and emotional rehabilitation that might be needed, patients may suffer a variety of late effects. A second malignancy may emerge because of a genetic predisposition, a side effect of irradiation or chemotherapy, or both. The growing and developing tissues of children are especially sensitive to therapeutic late effects. Neuropsychological disorders may emerge in children given brain irradiation and chemotherapy for brain tumors or acute leukemia. Radiation therapy and chemotherapy can also cause sterility, hypothyroidism, and cardiopulmonary dysfunction, as well as other functional disorders that may appear a few years or decades after therapy. Patients and their family physicians should be made aware of such possibilities and encouraged to be diligent. They need a physician who is hopeful, truthful, compassionate, understanding, accessible, informative, and knowledgeable. Although cancer patients understand that several physicians and other professionals will be involved in their care, they prefer and need one physician who can assume ultimate responsibility for their myriad needs. Patients should be told of plans and procedures in language that is understandable and appropriate. Because the weeds cannot be removed manually from the marrow, chemicals are used to destroy the weeds and allow the crops to grow. Physicians and family often mistakenly believe that the patient is concerned only with the possibility of death. In fact, patients are often equally or more concerned with the immediate implications of disease, for example, separation from family, pain, disfigurement, lengthy hospitalization, financial ruin, or missed time at work or school. Some patients and families become very knowledgeable about the disease and may know as much as or more than physicians about certain details; this knowledge should be viewed as an asset that can aid the physician in management. Physicians, nurses, and other caregivers may become emotionally attached to a patient or the family; this attachment need not be avoided if the necessary professional relationship and sound medical judgment are sustained. The physician must realize that, above all, the patient and family want an expert physician, not a pal or buddy. When the cancer becomes resistant to therapy and death is imminent, the patient and family need support more than ever to help them through the last days. The family must understand that no known effective therapy remains and that the goal of management must change from destroying cancer cells to providing comfort. Once this decision is made, chemotherapy, transfusions, antibiotics, blood cell counts, and other laboratory tests are no longer necessary. The patient should be hospitalized only if proper supportive care or pain medication cannot be given at home. For pain that cannot be controlled by oral analgesics, parenteral morphine is the drug of choice and is most effective when given by continuous intravenous infusions, which can be self-regulated (see Chapter 27). The demonstrably unwarranted fear of narcotic addiction, the rigid adherence to timed dosages irrespective of need, and the lack of knowledge and human insensitivity of doctors and nurses are widespread and indefensible. There is no reason for any cancer patient to suffer severe unremitting pain, a consequence of cancer more feared than death by most patients. Terminally ill patients themselves seldom ask the physician whether they are going to die, probably because they already know or suspect the truth and do not want to confront the physician with an uncomfortable question. Should the question be asked, however, the patient probably knows the answer already; to deny the truth is worse than useless. Although guidelines can be provided for the caring of patients during this difficult period, the medical staff must adopt an approach that is suitable to the particular patient and circumstances. Most of all, the patient needs palpable demonstration that the medical staff is readily available and willing to listen, to comfort, to provide any possible service, and simply to be there.
Transfused lymphocytes engraft gastric bypass diet buy 800mg renagel overnight delivery, recognize gastritis diet àáâ discount 800 mg renagel overnight delivery, and react against the host (recipient) gastritis empty stomach 400 mg renagel mastercard. Hence chronic gastritis malabsorption order renagel with a mastercard, prevention is a primary goal and is accomplished by subjecting blood and components to 25 to 30 Gy gamma irradiation. Endocrine, cardiac, and liver dysfunctions occur in adults who receive 60 to 210 (mean, 120) units of blood. Iron chelation therapy or possibly exchange transfusion reduces iron stores or iron accumulation. This infrequently occurring syndrome is manifested by profound thrombocytopenia 5 to 9 days after transfusion. Primary therapy involves intravenous gamma globulin infusion; plasma exchange is an alternative. Some studies report a higher incidence of postoperative infection in transfused than in non-transfused patients. Although the data are conflicting, it appears that the use of leukocyte-reduced blood components reduces this putative immunomodulatory effect. Available evidence provides less support for concluding that patients with malignancies given transfusions in the perioperative period have a greater recurrence rate and lower survival rate than non-transfused patients. Significant improvements in donor screening and laboratory testing procedures lessen the risk. Transfusion-transmitted hepatitis A infection occurs infrequently because few donations are made during the asymptomatic viremic phase. Currently, the risk of transfusion-associated hepatitis B per unit varies between 1 per 63,000 and 1 per 233,000 units. The risk of hepatitis C infection after transfusion relates to the 70- to 82-day "window period" between infection and detection of hepatitis C antibodies. Infectivity occurs during this interval with the resultant risk of hepatitis C infection per unit of approximately 1 per 103,000 to 121,000 units. These viruses reside intracellularly in leukocytes and, therefore, transfusion transmission is linked to cellular components. The interval between exposure and antibody detection is approximately 51 days; the risk per unit is 1 in 640,000. This latent virus, present in polymorphonuclear leukocytes and lymphocytes, rarely causes symptomatic illness in immunocompetent patients. The incubation period after transfusion ranges from 7 to 50 days (average, 20 days). The risk of this complication is reduced by not accepting blood donations from persons who have traveled to or emigrated from endemic areas. Trypanosoma cruzi, transmitted by transfusion, may cause fulminant illness in immunocompromised patients. Preliminary studies in the United States, involving follow-up of recipients of donations made by persons with environmental or serologic evidence of T. Further evaluation is required to determine the risk of transmitting this agent by transfusion. Transmission of this disease by blood or plasma derivatives has not been reported. However, cases have been linked to iatrogenic events such as exposure to contaminated human pituitary-derived growth hormone and dura mater transplants. Animal model experiments suggest transmission requires the presence of B lymphocytes. Other infectious agents that are transmitted infrequently by blood transfusion include Babesia, Bartonella, Epstein-Barr virus, and Toxoplasma. Transfusion of 1 unit of red cells increases the hemoglobin concentration by 1 g/dL and the hematocrit by 3%. The decision to transfuse red cells rests with a careful clinical assessment of the effectiveness of compensatory mechanisms for maintaining tissue oxygen delivery. A pre-set hemoglobin/hematocrit level should not be the sole reason for ordering transfusions. Patients without pulmonary, cardiac, cerebrovascular, or peripheral vascular disease tolerate a hemoglobin concentration of about 8 g/dL (range, 7 to 10 g/dL) without symptoms other than decreased capacity for activity. Patients with impairment of critical organs or tissues may require transfusion at higher hemoglobin/hematocrit levels. When prescribed, transfusions should be given on a unit-by-unit and case-by-case basis.
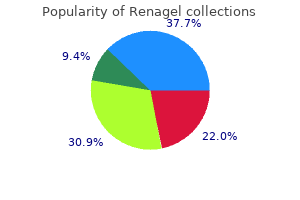
Aminosalicylates reduce the incidence of recurrences in patients with ulcerative colitis; almost all patients 727 Figure 135-3 Treatment algorithm for ulcerative colitis gastritis diet ëó÷øèå discount renagel 800 mg line. The efficacy of sulfasalazine at 3 to 4 g/day is greater than the efficacy of 2 g/day even though 2 g/day is the usual recommended maintenance dose gastritis diet xone buy discount renagel 800mg line. Response to therapy is monitored by empiric clinical assessment directed at the problem that is most troublesome for the patient chronic gastritis operation order 800mg renagel with amex. Patients with severe pain and diarrhea may have minimal findings on endoscopy or radiographic studies gastritis diet õàíóêà 400mg renagel sale. Patients who have undergone ileal resections may have significant diarrhea on the basis of their surgery alone. Prednisone is the drug of choice for patients who have failed to respond to aminosalicylates or metronidazole, for patients with ileal disease, and for patients with highly active colonic or ileocolic disease. For patients who have been brought into clinical remission on corticosteroids, the rate at which the dose is tapered is arbitrary and not defined by controlled trials. Usually the prednisone dose can be tapered from 40 mg/day to 20 mg/day relatively rapidly (5-10 mg/1-2 weeks) without inducing a flare of disease activity. Once the dose of prednisone has reached 20 mg/day, the taper is slowed to 5 mg every 10 to 14 days; if symptoms flare, the dose of prednisone is increased. Approximately 60% of corticosteroid-dependent patients will be able to withdraw from corticosteroids using this approach; the alternative is surgery if there is a stricture or a focal area of involvement. The patient is hospitalized, given nothing by mouth, rehydrated with intravenous fluids, and given parenteral corticosteroids. Patients who respond to parenteral corticosteroids are switched to high-dose oral corticosteroids (prednisone 40 mg/day), and the dose of prednisone is gradually reduced. Twenty to 25 per cent of patients with extensive ulcerative colitis eventually undergo colectomy, usually because their disease has not responded adequately to medical therapy. Emergency colectomy may be required in toxic megacolon or in a severe fulminant attack without toxic megacolon. The most popular alternative operation is the proctocolectomy and ileoanal anastomosis; in this procedure, a pouch is constructed from the terminal 30 cm of ileum, and the distal end of the pouch is pulled through the anal canal. The risk of developing malignancy enters into the equation when considering colectomy in those with long-standing ulcerative colitis; if the other indications are equivocal, the risk of malignancy may push the balance in favor of colectomy. Surgery is also performed to allow patients to stop taking medications (usually corticosteroids). The incidence of recurrence severe enough to need repeat surgery after ileal or ileocolic resection is about 50% after 10 years and 75% after 15 years. Physical examination may reveal postural hypotension, tenderness over the distribution of the colon, and absent or hypoactive bowel sounds. Antispasmodics and antidiarrheal agents are likely to initiate or exacerbate toxic megacolon. Medical therapy is designed to reduce the likelihood of perforation and to return the colon to normal motor activity as rapidly as possible. Intravenous fluids should be administered to replete water and electrolytes, broad-spectrum antibiotics are given in anticipation of peritonitis resulting from perforation, and parenteral corticosteroids are given at a dose equivalent to more than 40 mg of prednisone per day. Signs of improvement include a decrease in abdominal girth and the return of bowel sounds. Deterioration is marked by the development of rebound tenderness, increasing abdominal girth, and cardiovascular collapse. If the patient does not begin to show signs of clinical improvement during the first 24 to 48 hours of medical therapy, the risk of perforation increases markedly, and surgical intervention is indicated. Leakage of intestinal contents through a fissure into the peritoneal cavity results in an abscess. Extension of the inflammatory process through the wall of adjacent viscera or through the abdominal wall to the exterior results in a fistula. The typical clinical presentation of intra-abdominal abscess is fever, abdominal pain, tenderness, and leukocytosis.
Hypoperfusion of the renal vasculature occurs frequently in shock gastritis and diet pills effective 400mg renagel, in part due to preferential direction of blood flow to the brain and heart gastritis peanut butter order 400 mg renagel visa. Initially gastritis full symptoms purchase renagel us, vasoconstriction may maintain glomerular perfusion gastritis diet àâàòàí renagel 800 mg otc, but when this compensatory mechanism fails, acute tubular necrosis and renal insufficiency occur. An important clinical challenge is to differentiate between acute tubular necrosis and hypovolemia, because both present with oliguria (see below). Gastrointestinal Tract and Liver Typical clinical manifestations of gut involvement during shock include ileus, erosive gastritis, pancreatitis, acalculous cholecystitis, and submucosal hemorrhage. Some studies suggest that gut barrier integrity may be compromised, leading to translocation of bacteria and their toxins into the blood stream. The most common manifestation of liver involvement in shock is mild increase in transaminases and lactate dehydrogenase. With severe hypoperfusion, shock liver may be manifested by massive transaminase elevations and extensive hepatocellular damage. With an acute insult that resolves, these transaminase elevations will peak in 1 to 3 days and resolve by 10 days. Decreased levels of clotting factors and albumin may occur and reflect decreased synthetic function. In septic shock, significant elevations of bilirubin may be seen with only modest transaminase increases because of dysfunction of bile canaliculi due to inflammatory mediators or bacterial toxins. Hematologic Thrombocytopenia can occur due to dilution during volume repletion or may result from immunologic platelet destruction, which is especially common during septic shock. Activation of the coagulation cascade can lead to disseminated intravascular coagulation, which results in thrombocytopenia, decreased fibrinogen, elevated fibrin split products, and microangiopathic hemolytic anemia. Immune System Widespread dysfunction of the immune system has been described especially during hypovolemic and traumatic shock. Abnormalities of function in macrophages, T and B lymphocytes, and neutrophils have been described. These abnormalities are not thought to produce immediate effects but may contribute significantly to late mortality, which is frequently due to complicating infection. Metabolic Early in shock, hyperglycemia usually occurs due to glycogenolysis and gluconeogenesis mediated by increases in adrenocorticotropic hormone, glucocorticoids, glucagon, and catecholamines as well as decreases in insulin. Later in shock, hypoglycemia may occur due to glycogen depletion or failure of glucose synthesis in the liver. Also, protein catabolism ensues, resulting in negative nitrogen balance; this catabolism may be an important determinant of late mortality in shock, and some studies suggest nutritional supplementation is important in shock therapy. In distributive shock, although a low cardiac output may occur infrequently due to inadequate preload or myocardial depression, most commonly a low systemic vascular resistance and maldistribution of blood flow lead to low blood pressure and shock despite normal or increased cardiac output. Hypovolemic Shock this form of shock is characterized by fall in ventricular preload, resulting in decreased ventricular diastolic pressures and volumes, decreased stroke volume and cardiac output, and reduced blood pressure. Patients manifest pale, cool, clammy skin; tachycardia; decreased jugular venous pulse; decreased urine output; and altered mental status. The severity of hypovolemic shock is clearly associated with both the magnitude and the rate of fluid loss. Acute loss of 10% of circulating blood volume results in tachycardia and increased systemic vascular resistance with maintenance of blood pressure. Compensatory mechanisms begin to fail with a 20 to 25% volume loss: mild to moderate hypotension and decreased cardiac output occur, systemic vascular resistance is markedly increased, and lactate production may begin. With loss of 40% of circulating blood volume, severe hypotension develops with signs of shock; cardiac output and tissue perfusion are severely decreased. If this shock state persists for more than 2 hours, sufficient tissue damage will have occurred so that adequate fluid repletion will no longer be effective in reversing shock; that is, the shock will be irreversible. If the volume loss is produced at a slower rate, the compensatory mechanisms are more effective, and similar amounts of volume depletion are better tolerated. Cardiogenic Shock Cardiogenic shock results from failure of the heart as a pump, due to myocardial, valvular, or structural abnormalities. Hemodynamically, ventricular filling pressures and volumes are increased; cardiac output, stroke volume, and mean arterial pressure are reduced. Patients manifest signs of peripheral hypoperfusion coupled with evidence of ventricular failure (see Chapters 47 and 95).
Order renagel 400mg otc. Hiatus hernia: signs symptoms and treatment.